Diabetes disease is a long-term condition that affects how your body converts food into energy. It involves problems with insulin production and use, which leads to high blood sugar levels. Insulin, a hormone made by the pancreas, helps glucose from food enter your cells for energy. When the body doesn’t make enough insulin or can’t use it properly, glucose remains in the blood, causing elevated blood sugar levels.

There are three main types of Diabetes Disease:
Type 1 Diabetes Disease
Type 1 Diabetes Disease is an autoimmune condition where the immune system attacks and destroys insulin-producing cells in the pancreas. This form of diabetes usually appears in children and young adults but can happen at any age. People with Type 1 diabetes need lifelong insulin therapy, regular blood sugar checks, and lifestyle changes to manage their condition.
Type 2 Diabetes Disease
Type 2 diabetes is a metabolic condition where the body resists insulin or does not produce enough of it. It is the most common type of diabetes and is often linked to obesity and inactivity. Managing it usually requires lifestyle changes, oral medications, and sometimes insulin.
Gestational Diabetes Disease
Gestational diabetes happens during pregnancy and can impact both the mother’s health and the baby’s growth. While it usually goes away after birth, it raises the chance of getting Type 2 diabetes later on. Managing it involves following a healthy diet, exercising regularly, and keeping track of blood sugar levels.
Symptoms of Diabetes Disease
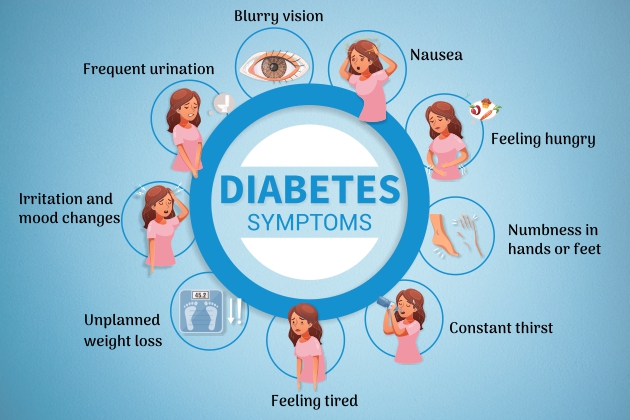
Recognizing the symptoms of diabetes early can lead to prompt diagnosis and treatment, improving outcomes and quality of life.
Early Signs and Symptoms
- Increased Thirst and Hunger: Ongoing hunger and intense thirst are typical signs of diabetes. Even with more food and drink, satisfaction may not follow.
- Frequent Urination: High blood sugar levels cause increased urination, often noticeable at night.
- Fatigue: Constant tiredness happens because the body can’t use glucose properly.
- Blurred Vision: High blood sugar levels can make the lenses in the eyes swell, leading to blurred vision.
Advanced Symptoms
- Slow-Healing Sores: Diabetes can reduce blood flow and nerve function, slowing the healing of cuts and wounds.
- Frequent Infections: Those with diabetes are more prone to infections, including those of the skin, urinary tract, and gums.
- Numbness or Tingling in Hands/Feet: High blood sugar levels can damage nerves, causing these sensations, known as neuropathy.
Causes for Diabetes Disease
Several factors contribute to the development of diabetes, including genetic, environmental, and lifestyle factors.
Genetic Factors
- Family Background: Having a relative with diabetes increases your risk of getting the condition.
- Genetic Factors: Certain genes can make someone more likely to develop diabetes, affecting how the body produces and uses insulin
Environmental Factors
- Lifestyle and Diet: Eating a diet high in sugar and fats, along with a lack of physical activity, significantly contributes to Type 2 diabetes.
- Physical Inactivity: Not exercising raises the risk of Type 2 diabetes by leading to obesity and insulin resistance.
- Obesity: Carrying extra weight, especially around the abdomen, is strongly linked to diabetes due to its effect on insulin sensitivity.
Other Contributing Factors
- Age: The chance of getting Type 2 diabetes increases as you get older, especially after 45.
- Hormonal Changes: Hormone shifts during pregnancy can cause gestational diabetes. Women with gestational diabetes have a higher risk of developing Type 2 diabetes later.
- Stress and Illness: Long-term stress and certain illnesses can cause diabetes by disrupting how your body makes and uses insulin.
Treatment of Diabetes Disease
Effective diabetes management involves a combination of medical treatments, lifestyle changes, and regular monitoring.
Medical Treatments
- Insulin Therapy: Crucial for managing Type 1 diabetes and sometimes required for Type 2 diabetes. Insulin can be given through injections or an insulin pump.
- Oral Medications: Various drugs help control blood sugar in people with Type 2 diabetes by boosting insulin production, lowering glucose production, or improving insulin sensitivity.
- Injectable Medications: Non-insulin injectables, such as GLP-1 receptor agonists, help regulate blood sugar by mimicking hormones that control glucose metabolism.
Lifestyle Changes
- Consistent Exercise: Physical activity aids in weight control, enhances insulin sensitivity, and reduces blood sugar levels.
- Nutritious Eating: A diet full of vegetables, whole grains, lean proteins, and healthy fats is essential for stable blood sugar levels.
Monitoring and Management
- Monitoring Blood Sugar: Checking blood sugar regularly is crucial for managing diabetes and avoiding complications.
- Routine Check-Ups: Regular visits to healthcare providers help track the condition and address any complications.
Advanced Treatments and Research
- New Medications: Ongoing research is creating new drugs to improve diabetes care.
- Technological Advancements: Insulin pumps and continuous glucose monitors (CGMs) help manage diabetes by giving more accurate blood sugar control.
- Ongoing Research: Clinical trials and studies work to find better treatments and possible cures for diabetes.
Diet for Diabetes Disease
A healthy diet is a cornerstone of diabetes management. It helps maintain stable blood sugar levels, supports overall health, and prevents complications.
Importance of Diet in Diabetes Disease Management
- Dietary Control: A balanced diet regulates blood sugar and supplies essential nutrients for overall health.
Key Dietary Principles
- Low-Carb Diets: Reducing carbs helps minimize blood sugar spikes.
- High-Fiber Foods: Fiber slows sugar absorption and improves blood sugar control.
- Healthy Fats: Including healthy fats supports heart health and general well-being.
Specific Dietary Recommendations
- Meal Planning: Organizing meals with proper carbs, proteins, and fats portions maintains stable blood sugar levels.
- Portion Control: Avoiding overeating is crucial for managing blood sugar and preventing weight gain.
- Balanced Diet Examples: Lean proteins, whole grains, and plenty of vegetables are staples of a diabetes-friendly diet.
Foods to Avoid
- Sugary Foods and Drinks: These cause rapid blood sugar spikes and should be limited.
- Refined Carbohydrates: Foods like white bread and pasta quickly raise blood sugar levels.
- Trans Fats: Found in many processed foods, trans fats are linked to increased insulin resistance.
Sample Meal Plans and Recipes
- Healthy Breakfast Ideas: Options like oatmeal with berries provide a balanced start to the day.
- Lunch and Dinner Options: Meals like grilled chicken with vegetables and quinoa are nutritious and satisfying.
- Snack Suggestions: Nuts, seeds, and low-carb options like cheese and vegetables make great snacks.
Conclusion
Grasping diabetes, identifying its symptoms, understanding its causes, and managing it through good treatment and diet are essential for a healthy life. By staying informed, consulting doctors, and making healthy lifestyle changes, people with diabetes can control their condition well and live satisfying lives.
Visit: Home Page
